Management of the Mandibular Deformity in the children with Craniofacial Microsomia
Treatment of the growing child
Correction of end stage deformities is usually done on older children and adults, but for certain malformations earlier intervention is encouraged.
ex: obstructive sleep apnea
Reason:
it would normalize the functional matrix, therefore improving the growth potential by placing strucures in a better anatomic locations. additionally, it will improve function, aesthetic and symmetry.
it would normalize the functional matrix, therefore improving the growth potential by placing strucures in a better anatomic locations. additionally, it will improve function, aesthetic and symmetry.
Treatment approach:
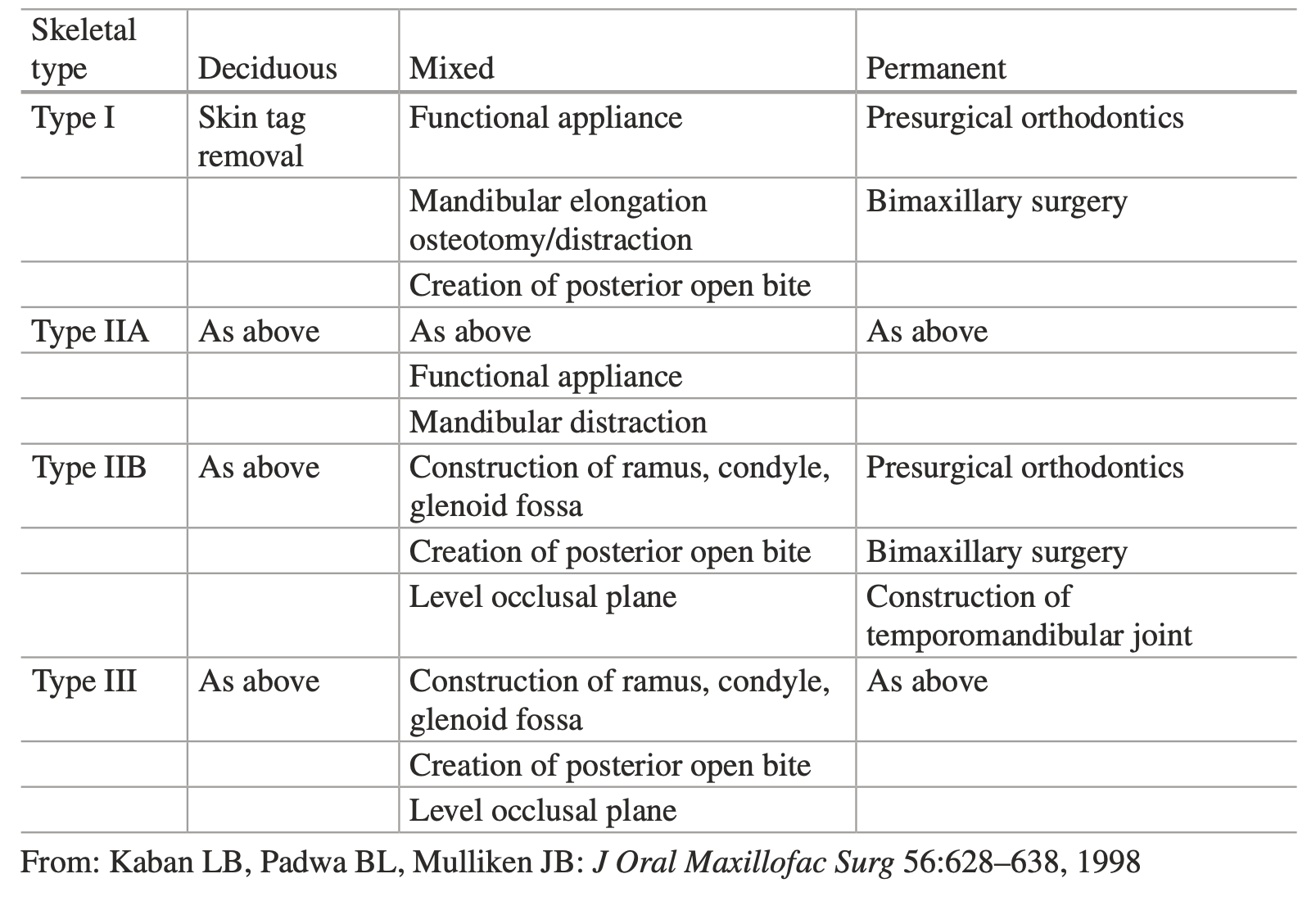
it's determined by the mandibular skeletal type (Kaban types I, IIA, IIB and III), presence of midface deformity, age based on chronical, dental and skeletal, and psychosocial development.
it's determined by the mandibular skeletal type (Kaban types I, IIA, IIB and III), presence of midface deformity, age based on chronical, dental and skeletal, and psychosocial development.
Treatment goal:
- Create an open bite surgically by elonagtion and rotation of the mandible to the midline
- Create an open bite surgically by elonagtion and rotation of the mandible to the midline
General assessment principles
by dentition and skeletal type:
Steps of the treatment
-
Functional appliance treatment
- It enhances the neuromuscular environment, promotes mandibular and maxillary growth, and expands the soft tissue envelope on the affected side.
- It holds the affected side of the mandible in a lowered and protrusive position.
- It stimulates bone apposition in the ramus-condyle unit and coronoid process by acting as the normal translatory and protrusive motion produced by the lateral pterygoid muscle.
- Indicated for patients with type I CFM.
- Good response to appliance therapy eliminates the need for surgical lengthening of the ramus.
- Reduces the tendency for postoperative skeletal relapse.
-
orthodontic treatment
- Focus is on control of tooth eruption.
- It prevents or corrects dentoalveolar adaptations to the asymmetrical position of the maxilla and mandible.
-
Mandibular Operation and Immediate Postsurgical Dental Appliance
- Indicated for type I, IIA, and some IIB patients.
- The mandible is elongated and rotated to the correct midline.
- Methods: conventional orthognathic surgical methods or by distraction osteogenesis (DO).
- Prevents the need for a Le Fort I osteotomy after completion of skeletal growth.
